
- 9Neonatal and Paediatric Surgery Laser Clinic at Perth Paediatrics (West Leederville)
- 9New Born Circumcision
- 9Laser Repair of Tongue Tie and Maxillary Frenulum (Lip-Tie)
- 9Paediatric General Surgical Clinic
- 9Complex Bowel Management Clinic at Perth Paediatrics (West Leederville)
- 9Do you have someone to refer?
PREHOSPITAL
DAY OF SURGERY
DISCHARGE AND REVIEW
FINANCIAL
POSTOPERATIVE EMERGENCY

We provide Laparoscopic ( key hole ) surgical services for number of …

We provide neonatal laser surgery for tongue tie,upper lip tie repair…

Paediatric gastroenterology Perth’s bowel management team includes paediatric…

For regional and rural paediatric patients, our doctors provide video…

Our services include management of inguinal/umbilical hernias…



Please note a valid referral from your GP or specialist is required.

The timing of orchiopexy surgery is 6-12 month’s age, and for inguinal testes the success rate in terms of scrotal position and lack of atrophy is 82-89%.
Diagnostic laparoscopy via an umbilical port is the procedure of choice in NPT – ultrasound can evaluate inguinal testis well but is not reliable for an intra-abdominal testis. The presence of blind ending vessels on diagnostic laparoscopy is the hall mark of testicular atrophy/anarchia (due to prenatal torsion)
A gastrostomy button is placed via a general anaesthetic with a keyhole technique. Children generally stay in the hospital for about 2-3 nights after the operation and during this time we will take the opportunity to teach you about the care and management of the gastrostomy button. It is generally important before the operation to get an idea as to whether or not your child has significant gastro-oesophageal reflux.
If there is severe gastro-oesophageal reflux or any of the complications of gastro-oesophageal reflux such as recurrent chest infections, oesophagitis, or so much vomiting that we are not able to get enough calories in, and then a consideration might be made for combining the placement of the gastrostomy with a Nissen fundoplication after thorough investigations. However, most children are able to cope with just a gastrostomy alone.

There are two common causes of gallstone disease in children and these occur in roughly equal proportions. The first cause is in children who have increased breakdown of their red cells such as in sickle cell disease, thalassemia, or spherocytosis. These diseases often run in families and so people already know about them. Because the red blood cells are being broken down at a higher rate the bilirubin that is one of the building blocks of the red blood cell can accumulate in the gallbladder causing bilirubinate stones. These stones can occur at any age even in very young children.
The second common cause of gallstones in children are cholesterol stones. There is often a family history of gallstones and it affects teenage girls more often than boys. Gallstones can present in a number of ways but usually present with abdominal pain. This pain can be central or right sided and some children describe the pain as going around to their back. It can be bought on by meals, especially meals with a high fat content. A number of children with gallstone disease already have very little fat in their diet. They avoid fat because they know that this can bring on the symptoms. More serious problems caused by gallstones is when they escape from the gallbladder into the common bile duct. Here they can cause an obstruction and the child may become jaundiced or they could cause an episode of pancreatitis.
A newborn who has Hirschsprung’s disease usually can’t have a bowel movement in the days after birth. In mild cases, the condition might not be detected until later in childhood. Surgery to bypass or remove the diseased part of the colon is the treatment
Recent trends in surgery for Hirschsprung’s disease ( absence of ganglion cells in bowel) have been toward earlier repair and fewer surgical stages. A one-stage pull-through for Hirschsprung’s disease avoids the additional anesthesia, surgery, and complications of a colostomy. A laparoscopic-assisted approach diminishes surgical trauma to the peritoneal cavity.
The technique uses three incisions on the abdomen. The transition zone ( between healthy and diseased bowel) is initially identified by seromuscular biopsies obtained laparoscopically.
- Ano means the anus. This is the opening at the end of the large intestine. Stool passes through here when there is a bowel movement.
- Rectal means the rectum. This is the part of the large intestine just above the anus.
Normally during a bowel movement, stool passes from the large intestine to the rectum and then to the anus. Muscles in the anal area help to control when you have a bowel movement. Nerves in the area help the muscles sense the need for a bowel movement. The nerves also stimulate muscle activity.
With an anorectal malformation, several problems can occur. These include:
- The anal passage may be narrow
- The anal opening may be covered with a tissue or membrane
- The rectum may not connect to the anus
- The rectum may connect to part of the urinary tract or the reproductive system. This happens through a passage called a fistula.
Anorectal malformations cause problems with how a child has a bowel movement. Treatment depends on which type of problem your baby has.
Anorectal malformation may be seen with some genetic syndromes or congenital problems that are present at birth. These include:
- VACTERL association. This disorder includes problems with the spine, anus, heart, trachea, esophagus, kidneys, and arms and legs.
- Digestive system problems
- Urinary tract problems
- Spinal problems
- Down syndrome
While low-type imperforate anus in most cases, low-typed malformation could be corrected by one-staged anoplasty but a temporary defunctioning colostomy usually required in intermediate or high-type malformation before the definitive repair. The difinative surgery can be performed with key hole surgery ( laparoscopic assisted rectal pull through (LARP)) Apart from being minimally invasive, LARP also possesses an advantage in the management of high-type malformation such recto-vesical fistula that would require laparotomy. The magnification property of laparoscopy also allows the accurate placement of the pull-through rectum.
Antegrade colonic enema surgery (ACE) or Malone antegrade colonic enema (MACE) is a procedure that is designed to help empty the bowel of feces. The procedure allows the emptying of the bowel by using fluid (similar to an enema) that is inserted into a small opening in the side of the abdomen rather than into the rectum.
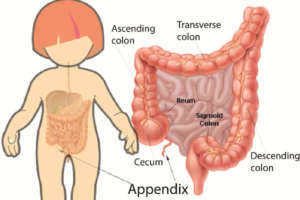
The reasons for the surgery include problems such as constipation and fecal incontinence. These problems may be caused by many conditions. They may be congenital (present at birth) abnormalities that affect the rectum and anus, or they can be caused by neuropathies (nerve supply problems) that result from spinal abnormalities.
ACE surgery is with performed with key hole when other methods to control constipation or fecal incontinence have not been successful. These other methods might include bowel training, dietary changes, medications taken rectally (suppositories or enemas), or medications taken by mouth.
Most people use their ACE once daily, but a few need to use it only every other day. An irrigation may take 30-60 minutes. It is important to stick to a routine and empty your bowels at approximately the same time every day. Approximately 30 minutes after a meal is a good time to empty the bowels, as the colon has increased activity and good clearance of bowels is more likely.
These operations may be performed by thorcoscopy through tiny incisions, depending upon the type of procedure and the size of the patient.

- Laser repair of tongue tie (up to 6 months of age)
- Laser repair of maxillary frenulum
- Laser circumcision up to 12 weeks of age
- Laser excision of umbilical granuloma/polyp
- Laser excision of mucosal/skin lesions
- Undescended Testis
- Inguinal/Umblical hernias
- Circumcision for cultural/ medical reasons( after 6 months)
- Penile problems including hypospadias
- Vascular malformations /Haemangiomas
- Head and neck lumps ( Lymphnodes, Thyrglossal cysts, branchial anomalies)
- Paediatric Gastrointestinal Clinic for constipation, Hirscsprung’s disease, anorectal disorders
- Thoracoscopic and Laparoscopic Surgery
- Tongue tie repair
- Anorectal disorders including encopresis and Intractable constipation in collaboration with gastroenterologist, dietician, psychologist and Continence physiotherapist.
- Real time ultrasound, anorexia muscle complex assessment and Anorectal manometry.
- Paediatric Gastrointestinal surgery including Hirschsprung’s disease.
