We have taken extra precautions by implementing the Australian Government Infection Control measures for COVID-19 such as hand hygiene and physical distancing for patients (where possible) and frequent disinfection of office equipment and furniture. Our team has undergone specialist COVID-19 infection control training. We are keeping up to date with all new information that is available.
If the passage stays open, fluid can pass from the tummy cavity and surround the testis. Even when there is a lot of fluid, it does not harm the testis in any way.
As the communication may close without an operation, we generally wait until the boy is about 18 months of age before recommending surgery. If the hydrocoele does not resolve by this age, an operation is advised as the fluidcollection may become uncomfortable for the boy as he becomes older.
Consistent with guidelines from The Royal College of Surgeons of Australasia we are limiting treatment to those which cannot be delayed, or which help reduce strain on hospital and primary health care providers. These include:
Frenectomies for infants with the below criteria:
Due to the risks associated with not breastfeeding / shortened breastfeeding duration, addressing restricted oral tissue is necessary and urgent
— Feeding difficulties
— Poor weight gain
— Breathing, swallowing (choking) or sleeping issues
— Maternal symptoms such as nipple trauma, mastitis or post-natal mental health challenges due to inability to feed.
POSTPONED TREATMENTS
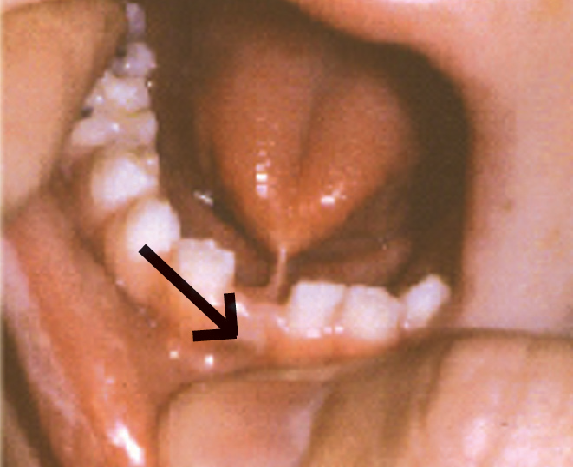
This is a piece of fleshy tissue running between the under surface of the tongue and the floor of the mouth. It is also called as the frenulum. The frenulum is present in most people but when thicker or shorter than normal it may restrict the movement of the tongue, particularly the ability to stick the tongue out of the mouth. A tongue tie may cause feeding difficulties, excessive drooling, and poor dental hygiene or be associated with speech problems.
In neonates and infants the procedure can be performed with scissors or Laser at Perth Paediatrics. The Laser procedure is performed with topical anaesthesia.Dr Gera has Clinical Nurse to assist the procedure at Perth Paediatrics.
PREPARATIONS FOR TONGUE TIE REPAIR UNDER GENERAL ANAESTHESIA
Your child will need to fast for solids and liquids generally for about 6 hours before the start of the procedure. In breast-fed babies or infants this time may be reduced after consultation with the anaesthetist. It is often helpful to bring your child’s favourite toy with you on the day.
ANAESTHESIA
You and your child will meet the anaesthetist on the morning of the procedure. After talking to you and briefly examining your child, they will take you through to the operating theatre. One parent is welcome to accompany your child until they are asleep. The anaesthetist puts your child to sleep via a face mask (with children 5 years and over there is the option of either a face mask or a needle with numbing cream).
PROCEDURE
The mouth is cleaned with a mild antiseptic solution. The tongue-tie is divided using an electrical cautery device, which both releases the tongue-tie and seals any blood vessels in the frenulumLocal anaesthetic is then applied in the form of a gel to the wound. The local anaesthetic block usually lasts around 2 to 3 hours.
INITIAL RECOVERY
Once the operation has fi nished, your child will be taken to the recovery area. Once awake, you will be called into the recovery ward. Often children appear mildly distressed and a little confused initially – there may be several reasons for this including residual effects of the anaesthetic, hunger and some discomfort. Generally they will settle quite quickly, especially if offered a drink or feed. The recovery and ward staff are also able to give pain relief medication once your child is awake and this is sometimes required. The nursing staff will check the wound and make sure you are happy before you go home. Usually this will be about 2 hours after the surgery.
As a result of the local anaesthetic nerve block, your child may complain of a numb sensation in the groin and in some cases some weakness in the leg on the side of the surgery. This is temporary and will generally settle within a day or so of the operation.
POST-OPERATIVE COURSE
Paracetamol (‘Panadol’) should be given on the afternoon and evening of surgery, and in the morning of the following day. After that time, assess your child’s pain to see if further doses are required. Older children may require a stronger medication such as ‘Painstop Daytime’ or ‘PainstopNighttime’ if over one year of age. Follow the manufacturer’s dose instruction but never give more than 4 doses in a 24-hour period and never both at the same time.
There may be a small amount of blood that oozes from the wound in the first 24 hours.
Your child can begin eating when they get home. Start with clear liquids (apple juice, iceblocks) and add solid food slowly and in small amounts. Your child may vomit from the anaesthesia on the day of surgery. This should stop by the morning after surgery.
Your child can begin eating when he gets home. Start with clear liquids (apple juice, iceblocks) and add solid food slowly and in small amounts. Your child may vomit from the anaesthesia on the day of surgery. This should stop by the morning after surgery.
RETURN TO ACTIVITY
Your child may return to day care or school when comfortable, usually within 3-5 days.
- You see any signs of infection: redness along the incision site, increased swelling, foul smelling discharge from incision
- Your child’s pain gets worse or is not relieved by painkillers
- There is bleeding (small ooze of blood in the first day or two is normal)
- Your child has a high temperature
- Vomiting continues on the day after surgery
- You have any questions or concerns
Follow up 4-6 weeks after surgery.
Follow-up
Normally, I recommend review in 6 weeks. Please note that although the wound generally heals very quickly, usually withing a week of the procedure, the scar at the floor of the mouth remains pale for several weeks or months. This will not cause any functional problems.
Problems & further surgery
Whilst surgical release of tongue-ties is usually uneventful, there is always a 2-3% risk of bleeding after surgery. Please also be aware that surgical release of a tongue-tie will not always be associated with an improvement in a child with an established speech impairment. Further assessment by your speech pathologist after the surgery is recommended.




